Liver is the second largest organ in your body.
It is located on the right upper side of your belly.
It weights approx. 800 grams to 1500 grams depending on person’s habitus.
The gallbladder, a storage bag for bile is attached under your liver.
Liver has two lobes, right lobe and a left lobe. If you go into microscopic level, each lobe is made up of smaller sections called lobules which are clusters of liver cells.
Let’s talk about major inflow and outflow of the liver.
There are two major vessels that goes into the liver.
First is Portal vein, which gets the unfiltered blood from small intestine carrying nutrients, medications, or toxins, sometimes infective bugs. and 75% to 80% % of liver blood flow is from Portal vein.
Second is Hepatic artery which brings oxygen rich blood into the liver. That brings 20% to 30% of total blood flow to the liver.
Three major vessels that come out from liver are right hepatic vein, middle hepatic vein and left hepatic vein. That drains into inferior vena cava, which is the largest vein in the body.
FYI, veins are the blood vessels that carry blood toward the heart.
Bile produced by the liver drains into the channel called Bile duct. These channels become bigger as they come out from Liver. Right and left hepatic ducts come together and form the common hepatic duct that eventually drains into your digestive system.
Bile usually stored in a bag called gall bladder, whenever system activated, it releases into first part of your small intestine.
By understanding why liver is important in your body, it will be obvious to you why you need a new liver when it fails.
You will never realize how hard your liver is working, all day, every day like other organs, because it’s not obvious. It performs more than 500 different vital functions.
I would like to divide in a three broad category.
Production Factory
It produces bile, various proteins for special functions, cholesterols, sugar, hormones.
Filtering Machine
It is the biggest filtering machine in the body. It filters more than a litre of blood every minute which is more than 80 litres of blood every hour and more than 900 litres of blood in a day. By filtering blood, it helps us fight infections and remove toxins from the body.
Storage House
It stores vitamins, minerals and sugar and release them as when required.
Remember, it is impossible to live with failed liver!
Liver is a very unique organ with special abilities!
It has enormous reserve. In simple words, you have more liver mass than you need to sustain life. It is very much possible to live a normal life with only 30% of your healthy liver.
It means two things.
you won’t have any signs and symptoms of liver disease or abnormal liver tests until very late into the course.
It allows us to do what we do as surgeons. we can safely remove up to 70% of liver in a case of either liver cancer or liver donation during transplantation without compromising liver function.
It has tremendous capacity to heal and regenerate. Unless the insult persists, it usually recovers without any issues. Liver usually grows back to its normal size within few weeks of donation during Liver transplantation.
As we know, Liver has a remarkable capacity to regenerate. Unless the initial insult persist, Liver heals itself. So, damage occurs when damage continues for a long time.
Liver failure happen either in acute, subacute and chronic form.
In acute form, liver fails in days to weeks’ time.
In subacute form, in weeks to months’ time.
In chronic form, Liver takes months to years to fail.
Many diseases may lead to chronic liver failure. Most common one’s are.
Viral hepatitis: Especially Hepatitis B and C.
Alcoholic Liver Disease- In my practice, Liver failure due to Alcohol is the most common indication for Liver transplantation.
Non-Alcoholic Steatohepatitis [N.A.S.H.] –
In NASH, there is a deposition of fat within liver cells which may result in inflammation and eventually fails the liver. People who are obese, diabetic, high lipid in their blood are the ones at risk for developing NASH. We are seeing increasing trend of NASH patients requiring Liver transplantation.
Autoimmune Liver disease- where destruction of liver happens by patient’s own immune system. More common in females.
Cholestatic Liver Diseases where destruction of channels which drains the bile from liver to gut called bile duct. It can be either Primary Biliary Cirrhosis or Primary Sclerosing Cholangitis.
Genetic Liver Diseases-
Hemochromatosis: excess iron deposition in the liver
Wilson’s disease: abnormal copper metabolism
Alpha-1 anti-trypsin deficiency: lack of a gene product that limits the activity of trypsin, an enzyme that digests protein. Over time this leads to progressive destruction of the liver and lung.
Glycogen storage disease (type I, III, IV): an inherited metabolic disorder
Tyrosinemia: a disorder of tyrosine metabolism
Vascular Liver Disease
Budd Chiari Syndrome- is clotting of the hepatic veins which lead to leads to liver failure, more common in female population.
Drug-induced Hepatitis- caused by certain drugs
Sometimes we do not find any reason for liver failure where we used the term called Cryptogenic Cirrhosis.
Liver diseases usually doesn’t show any signs or symptoms until late in its course.
So instead being worried about it, you should do regular health checks to avoid unnecessary delay in diagnosing liver diseases. Because many Liver diseases in initial stages can be reversed, controlled or treated.
When you meet your liver specialist, in your initial assessment you should expect,
Proper history and physical examination
Blood tests called Liver tests along with other routine tests
Sonography of Liver
To reach to a conclusion.
We usually do blood test called Liver Function test which includes measuring liver enzymes, special proteins and bilirubin in the blood.
Liver enzymes includes Alanine Transaminase (ALT), Aspartate Transaminase(AST), Alkaline Phosphatase (ALP), Gamma-glutamyl transpeptidase (GGT). Abnormality in these enzymes suggest there is an underlying injury to the Liver.
Special proteins are Albumin, Globulin, prothrombin.
A bilirubin test measures the level of bilirubin in your blood. If your liver is damaged, bilirubin can leak out of your liver into your blood and can cause yellowness of skin and eyes.
We also do other specific blood test depending on suspicion.
Common imaging used in diagnosing liver diseases are Sonography, CT scan and MRI. These test not able to tell us how stiff or fibrosed your liver is. So for that we use either Fibro scan which is a modified ultrasound machine or MR Elastography.
Finally, Liver Biopsy is the best way to learn more about disease affecting your liver. It can diagnose wide variety of liver diseases and stage one is in. It can also diagnose infections and cancers.
One of the most commonly asked question in our practice.
First of all, you should maintain healthy life style in general. Do all the good things.
Eat healthy
Excise regularly
Keep your weight in check.
Avoid alcohol, smoking and other recreational drugs.
Do Regular health checks to avoid unnecessary delay in diagnosing liver diseases. Because many Liver diseases in initial stages can be reversed, controlled or treated.
Get vaccinated as per your doctor’s advice.
Have safe sexual practices.
Use over the counter medications judiciously.
What is best for your body is best for the liver. There is nothing like a liver diet unless you are having a liver failure already.
Let me tell you one thing, no diet in the world will help you if you are not discipline and leading unhealthy lifestyle.
Now a day, it is nearly impossible not to indulge in one or the other unhealthy habits. I would suggest whatever you do, do it in moderation, be aware about your choices.
Avoid Junk or fast food whenever possible.
Avoid high fat, high sugar or high salt diet.
Best thing is not to drink. If you can’t avoid it then know your limits.
Try to incorporate wide variety of vegetables, fruits, grains, milk & its product, eggs, fish depending on season and geography you live in. Try to find a balance in your diet.
And last do not forget to hydrate yourself.
Remember, It’s not always about what you eat, it’s about how you eat and how much you eat. Work on it.
By definition, Cirrhosis is irreversible scarring of the liver which can be fatal.
Liver has a remarkable capacity to regenerate, unless the initial insult persist liver heals itself. So Liver cirrhosis occurs when damage continues for a long time
It can be in form of continuous alcohol abuse, various chronic viral infections, drugs, sometimes herbal medications, excess iron or copper in the liver or prolonged blockage of biliary system.
Initially, Patients with Liver Cirrhosis present with tiredness, lethargy, yellowness of skin, eyes and urine (mild jaundice), swollen feet, excessive itching and anemia (low hemoglobin).
In more advanced stages, the patient may have several life threatening complications such as blood vomiting, fluid in their belly, bleeding tendency, serious infections, mental confusion & coma, various other organ dysfunction like kidney, heart, lungs.
One cannot see or feel any symptoms of liver failure until very late in their disease course. It is a very good idea to see your family physician and do regular health check-ups.
Initially, people with liver disease or liver failure may experience: Tiredness, weakness, lethargy, nausea, vomiting, yellow colour of the skin and eyes, dark urine, pale stools, black stools, fluid in their belly, muscle cramping…and so on.
During later in the disease process they have more serious and life threatening symptoms requiring multiple hospital admissions like
Mental confusion and coma
Blood vomiting
Serious infections in the body
Internal bleeding
Kidney failure due to liver, may require dialysis
There is an exhaustive list of symptoms but you may not experience all the symptoms as I described.
It really dependent on what stage of cirrhosis you are in which usually defined by classification called child Pugh Turcott classification.
Cirrhosis is an irreversible process and continue to worsen if initial insult is there. For example, you continue to drink after having diagnosis of Cirrhosis.
So early cirrhosis (which includes child’s A or child’s B) can have fairly normal life for years provided patient is in a continuous follow up with their Liver specialist.
Advanced or Child’s C Cirrhosis on the other hand, required urgent intervention in the form of liver transplantation.
Straight answer, No, there is no medication that can prevent or reverse damaged liver/liver cirrhosis.
In early stages of liver damage, if you are able to catch the diseases which are treatable then it is possible to prevent progression and reverse the disease process. Thanks to liver’s enormous regeneration capability.
In later stages, to some extent you can decrease the symptoms caused by the liver failure.
Like, you can have water pills called diuretics to remove access water from the belly, per se it has no effect on liver what so ever.
You can take drugs to reduce or prevent mental confusion and coma.
And so on.
But one cannot heal the liver by medication So liver transplantation is the only permanent cure in advanced liver cirrhosis.
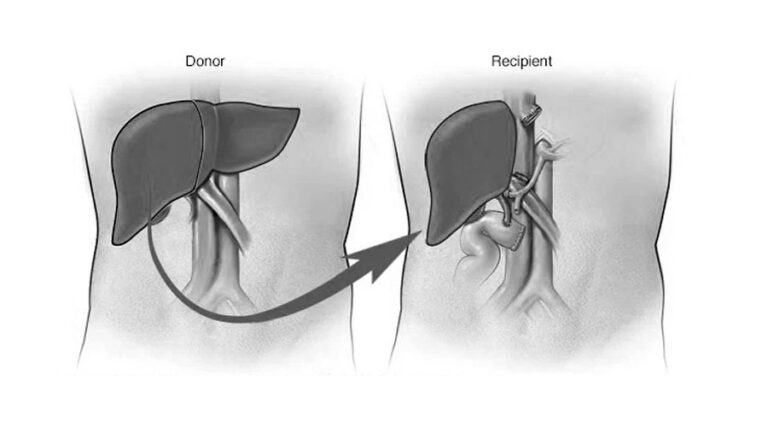
A liver transplant is a complex surgical operation to replace a failed liver with a new healthy one that comes from another person’s body.
You can receive a whole liver from a donor who has recently been pronounced brain dead, or
you can receive a part of a liver from a living donor.
At this time, transplantation is the only cure for end stage liver failure patients because no device or machine reliably performs all the functions of the liver.
Liver transplant is a last resort treatment. You may be needing liver transplant because you are having one of two conditions.
You are having liver failure in either acute or chronic form.
Or
You are having primary Liver Cancer called Hepatocellular carcinoma which is within specific criteria to undergo Liver transplantation.
You may say why
First is your liver is failed and you can’t survive without a functioning liver. At this time, there are no device or machine reliably performs all the functions of the liver.
If you want to live longer with improved quality of life than, Liver transplant may be the only option given current situation.
Well, you cannot avoid liver transplant completely but you can delay it by months or years depending on what type of liver disease you have and what stage you are in.
As a liver specialist, we use certain scoring system or classification to define severity of liver disease and predict short as well as long term mortality depending on your clinical condition and blood reports.
If you have acute liver failure, you may recover, but this can’t be predicted. Those who don’t recover may die within days.
Chronic liver failure is a more gradual process. People can live with cirrhosis for months or years before they need liver transplant. They may require it sooner if complications develop during the course.
Remember,
At this time, transplantation is the only cure for end stage liver failure patients because no device or machine reliably performs or replaces all the functions of the liver.
Overall, Liver transplant can save and improve quality of life.
Let’s start with where…
If you see, liver transplantation in India currently happening in a corporate hospital like us as well as few government hospitals and trust hospitals.
So if you decide to get it done in a government set up then definitely cost will be much less than a corporate hospital.
But, things to consider before you jump into conclusion are.
Urgency of transplant – how sick are you
Type of transplant – living donor vs cadaver donor
Is patient being a kid or adult?
Financial status
Logistics of transplant of a particular center
Let’s discuss how,
Each state in India has different policy to help their fellow residents. Please inquire more about benefits you can avail depending on state you are living in.
Apart from that, there are many NGO and Trusts working for a cause in the field of liver transplantation.
So, it is possible to raise funds towards transplantation.
Last option is online crowd funding platforms like Impact guru, Ketto that can help raise money for transplant. Liver transplant as a treatment of end stage liver failure patients has gained significant acceptance in last two decades.
It is estimated that 200,000 patients die of liver failure or liver cancer annually in India. About 10-15% of which can be saved with a timely liver transplant. So 25k-30k liver transplants are needed annually in India but only about 2000 transplant are being performed.
Because of gross mismatch in demand and supply of organs, currently 80% of transplants in India are from living donation. Most of the transplants are still being done in private sector hospitals.
Let me tell you, not all patients requiring liver transplantation are eligible for it. Each patient is evaluated for suitability vigorously as per centre’s protocol.
Assessment are focused on two areas.
First is confirming end stage liver disease which is not possible to reverse by any means and liver transplant is only option to improve survival and quality of life.
Second is patient’s ability to tolerate anaesthesia and surgery safely.
Goal of any transplant center in the world is to do transplant as safe and as successful as possible.
Sometimes during your transplant evaluation process, we identify problems that makes transplantation not an option for you.
Like
Severe heart or lung disease not amenable to liver transplant
Sever infections or ongoing sepsis
If you have cancer that has spread already outside liver or certain cancer in liver itself like cholangiocarcinoma.
Severe coma or questionable mental status
There are other factors that may disqualify you as a candidate are
Lack of family or social support
Financial issue
Active or ongoing alcohol abuse
Compliance to medications
The objective of transplant evaluation process is to determine if you are a transplant candidate or not. That also ensure that you can tolerate emotional as well as physical stress of the operation.
Your assessment includes extensive medical tests and consultations with different specialists.
Various Blood tests
Chest x-ray
EKG
Stress test or DSE for heart
PFT for lungs
Ultrasound, CT scan or MRI
Urine test
Gastroscopy or colonoscopy
Consultations
As part of the assessment process, you will meet
Transplant surgeon
Liver medical doctor also called Hepatologist
Transplant Coordinator
Anaesthesiologist
Medical Social Worker
Psychiatrist
Kidney doctor
Heart doctor
Lung doctor
OB-GYN doctor
Once we have the reports and consultation, multidisciplinary team decides that you are a candidate or not for Liver Transplantation.
Once you are diagnosed with liver cirrhosis and requiring a liver transplant, next questions comes is how can I get a new liver to replace the old one?
There are two sources where you can get a new liver.
First is brain dead donor where person’s heart is still beating and so rest of the organs functioning normally but brain is died due to severe brain injury. After careful screening of the donor, organs are allocated to those who are in need according to organ allocation policy of a particular state or country.
Second is one of the family member decide to give part of his/her liver to loved ones.
One major difference I can think is type of organs being transplanted.
I mean cadaver vs living related
Most of the western countries have a very well organised and run organ donation network, that’s why most of their transplants are cadaver liver transplants.
In 2021, US performed more than 9000 liver transplants, among them less than 5 percent were living related transplants.
Over the years we were not able to increase organ donation activity despite government and NGO efforts so donation rate is still dismal in most part of the countries except few states.
That’s force us to perform more living related transplants, our 80 % of total transplants are living related. But still there is a gross mismatch in demand and supply of organs in both side of the world.
It depends on what is the source of the Liver.
In cadaver donor, most of the time you will get a whole liver.
In Living donor, you will receive a part of the liver. Which part depend on multiple factors.
Before we go into more details, you should know the segmental anatomy of the liver. Liver made up of 8 segments which allow us to create different sizes graft depending on recipient age, weight and other factors.
In general, most adult will require right lobe that is segment 5, 6, 7, 8. that is approx. 60 to 70 of the adult liver.
On the other hand, kids only need 20% to 25% of the adult liver, which is left lateral segments (Made up of segment 2 & 3). Some older kid may require left lobe which segment 2, 3 and 4.
Here I want you to understand how waitlist is ranked, in other words who will get the liver whenever there is a donor.
In general, sicker patients get the liver first.
Someone who is having acute liver failure where liver fails within days
In some cases, kids if liver is suitable.
Rest of the patient pool, ranked according to MELD Score.
MELD Score is Model for End Stage Liver Disease Score which is a formula includes your level of bilirubin, creatinine, prothrombin time and sodium.
Higher the score, better is the chances to get a liver.
In kids, we used PELD score for the same.
Apart from MELD points, some patients are eligible to get exception points. Please consult your doctor regarding this.
I understand that it is very important decision to make when it comes to deciding a hospital or surgeon. But I cannot emphasize enough about importance of comprehensive experienced team to have the best outcome.
You have to understand that liver transplant is not a one-person job. You usually don’t get to know lot of other people who are involved.
Team usually consist of
Transplant Surgeons, Transplant Hepatologist, Liver Anaesthesiologists, Adult Intensivists, Paediatric Intensivist, Coordinator, Fund raiser, Medical Social worker, Psychologist, Psychiatrist, Financial advisors, ID specialist, Dietitian, Physiotherapist, and other supportive staff.
You should raise this questions when you visit any Transplant Centre for consultation. Because
Your outcome depends on how comprehensive and experienced your team is.
Always choose your team wisely!
Let’s discuss list of professionals involved in your transplant process.
It may be overwhelming to know and meet different health care providers in your first visit. These are the list of team members you may have to deal with during your transplant process.
Transplant coordinators are your one point of contact for all your queries during the process. They provide you with initial education, explain transplant evaluation process and helps you get you through the transplant in general.
Transplant surgeons are the ones who actually perform the transplant operation. They will explain you regarding importance of having a surgery, risk involved, possible complications and recovery process.
Transplant Hepatologist: are the ones who are trained to diagnose and treat diseases related to Liver in both paediatric as well as adult population. They will decide whether you need a transplant or not and manage your complications related to cirrhosis of liver.
They also involved in post-transplant care.
Liver Anesthesitists – specialized in giving anaesthesia to sick cirrhotic patients.
Critical care specialists are the ones who will take care of you during your ICU stay. Again you have adult and paediatric Intensivist.
MSW – Medical social workers is the person who will help you understand the legal requirement of transplant process, guide you to get the required documents and get the clearances from hospital authorisation committee and state authorisation committee whenever needed.
Fund raiser – will help and guide you raise the funds from different sources if you cut short on finances.
Financial counsellor– will explain you regarding total cost of transplant and insurance coverage.
ID specialist– are the physicians who are specialized in Infectious diseases who will help you throughout the transplant process, right from prophylaxis to treating infection during and after transplant.
Dietitian– will assess your diet and give nutritional education though different phases of your recovery.
Physiotherapist – will provide you counselling before and after transplant to rebuild your strength and flexibility.
Psychiatrist – will evaluate in depth about your mental state, insight, support network and more.
Apart from that you will require support from other specialities like radiology, transfusion medicine, microbiology, pathology
And backbone of any program are Physician assistants and Trained nurses in OR, ICU and Floor.
As a surgeon, let me tell you one thing for sure, without support of rest of the team, it nearly impossible to get best outcomes.
Always choose your team wisely!
If you have opted for cadaver donor liver transplantation and you are on the wait list, then this is what you should expect.
You may get a call any time depending on your clinical condition and MELD score.
Most of the time you will get a call in the middle of night. Once you get a call regarding liver offer and you say yes, then you have to go to hospital and get the basic blood work done depending on centre’s protocol.
There are two separate operations. One is donor surgery and second is actual transplant operation.
Donor surgery usually happen in another hospital where part of the surgical team physically goes there, do the operation and assess the quality of the organ, get the organ out and come back.
Once the recipient team get the go ahead signal from the donor team, you will be taken to the operation theatre. Anaesthesia team will put you to sleep. Your old liver and gall bladder will be removed first during the surgery to make room for the new liver. Then the new liver is transplanted. New connections are made between arteries, veins and bile duct. During this process, you may bleed because of complexity of the operation and disease you have.
When surgery is complete, your belly is closed with staples. We usually place a drain in your abdomen to remove excess fluid in initial few days to weeks. Surgery last 8-12 hrs.
You will be spending couple days in ICU depending on the clinical condition and week time on the floor. Most of the patient usually discharged within two weeks of time.
As you know that organ donation rate is very dismal in most part of the country except few states. So there is a long wait time and uncertainty of getting a cadaver liver.
On other hand, living related transplant can be a better choice. Because
No wait time.
Surgery can be done before patient become too sick.
Surgery is scheduled and planned
Patient will get better functioning liver as outcomes are better or equally good when compared to brain death donor.
Remember, Earlier the transplantation, better the outcomes!
Liver cancer also called Hepatocellular carcinoma (HCC) is a cancer that developed into the liver usually in the setting of liver cirrhosis due to various reasons.
Let’s take a couple of scenario…
For example, very small single tumor can be burned with ablation.
In a normal liver- tumor involving one or the other lobe, can be treated surgically by removing part of the liver.
Not all liver tumour can be cured with liver transplantation. Only a subset of population can be eligible for transplantation. Like small early liver cancers confined to liver, not spread outside the liver.
Widely accepted criteria for selecting patients for transplantation is Milan’s criteria which are based on number and size of tumors.
one tumour < 5cm or up to three tumours each < 3cm.
We can achieve up to 80 % cancer free survival in these select group of patients.
It does not mean that tumors outside these criteria cannot be considered for transplantation, but results obviously inferior compared to Milan criteria.
Other criteria used are UCSF criteria. Definitely, in select group of patients, transplant can be a curative option.
Transplant operation
Generally, a liver transplant procedure for recipient whether its living donor or cadaver donor follows this process:
Once you are in operation theatre, you will be put to sleep, the anaesthesiologist will insert a tube into your lungs to get you on machine breathing. Various lines will be inserted to give fluids, drugs, blood products and monitor your vital parameters during the surgery. A catheter will be put into your bladder.
Now Surgeon will open your belly after making a cut. And then will carefully separate the deceased liver, attached arteries and veins will be clamped to stop blood flow into the diseased liver and it will be taken out to implant the donor liver. The method used will depend on your specific case.
The donor liver will be attached to your blood vessels. Blood flow to your new liver will be started. The surgeon will check for any bleeding where you have stitches. The new liver will be attached to your bile ducts. The incision will be closed with stitches or surgical staples. A drain may be placed in the incision site to reduce swelling.
Recovery from liver transplant
After successfully completion of the operation, you will be shifted to Transplant ICU with the breathing tube and sedation.
Next couple of days you will stay in ICU until your condition stabilizes and your blood pressure and breathing are well controlled, and you are off the ventilator.
Then you are shifted to floor where you will continue to recover, gain strength, and learn how to manage with your organ transplant.
Most of our patients go home within two weeks after surgery.
Post-transplant Complications
can happen during the surgery as well as during your hospital stay post-transplant. We usually keep close eye on number of possible complications common during first two weeks.
The liver transplant may fail to function immediately after the transplant – this is called primary non-function (PNF), and is extremely rare (<0.5%). This may require another transplant to be performed very urgently.
Blood clots may form in arteries or veins carrying blood to the new liver (vessel thrombosis). This is very rare (1%), but may severely damage the new liver if it cannot be corrected immediately by surgery or blood thinners. In some cases, another transplant may be required because of this.
Internal bleeding may occur and may require blood transfusion or surgery (<5% risk).
Leakage of bile may occur from the connection between the new liver’s bile duct and your bile duct or bowel (10-20% risk). This may require surgery or placement of a drainage tube by the radiologist.
Narrowing or stricture of the bile duct after liver transplant may cause a problem with bile flow which may require surgery or placement of a stent by a radiologist or gastroenterologist (10-20% risk).
Acute rejection of the liver transplant may occur and can almost always be treated with medications to further suppress the immune system (15% risk).
Other complications that can occur to any patient having major surgery are also possible, including:
Cardiovascular problems such as heart attack, arrhythmia, or stroke
Kidney failure
Neurological problems such as seizures, tremors, or confusion
Respiratory problems such as pneumonia or pulmonary embolism
Infections of the surgical wound, IV sites, or urine.
Yes, wherever there is a skin cut that heals and leaves a scar.
Donor usually has reverse L scar in upper part of the belly. If it is done laparoscopically, then you won’t see a scar over period of time.
In recipient, scar size and type depend on multiple factors.
Age of the patient
Type of transplant being done
But in general,
Kids, usually get horizontal scar in upper belly.
Adults usually have reverse L or Inverted T depending on the particular case.
Liver transplant in general improve survival and quality of life.
There are few subtle changes that happen after transplants are
Your energy level improves
You can have normal diet, there won’t be any restrictions
No fluid restriction as you used to before transplantation
Your memory improves
Overall, your life returns to normal.
As such there are no disadvantages to liver transplantation, there are certain things that comes with a new liver.
First is you have to take lifelong medications called Immunosuppressant’s regularly in order to protect your liver.
You have to maintain lifelong follow up to transplant team.
You may have side effects from medications that you are taking.
You have higher chances of having infection and certain type of cancers than general population.
The risk of infection related to transplantation needs to be considered when choosing whether or not to proceed with liver transplantation.
Infections are an unavoidable risk of transplantation. They are the most common complication after transplantation, occurring in about 1/3 of patients. The risks of developing an infection must be balanced against the benefits of a transplant.
Transplant patients are at greater risk for infection because the anti-rejection drugs given after transplant affect their immune systems. Bacteria, viruses, fungi, or other organisms can cause infections. Most infections can be successfully treated, but some are difficult to treat and can cause disability or death.
Wound infections, abscesses, pneumonia, and urine infections are potential complications of any surgery. Some of the common infections are… MDR Bacteria, CMV, Hepatitis B & C, Epstein Barr Virus, other unknown Infections.
Some liver diseases that were present before transplant, and caused the need for transplant in the first place, may recur in the new liver graft.
Like Hepatitis B, Hepatitis C, Non Alcoholic Steatohepatitis, Autoimmune liver diseases, Hereditary Liver diseases,
Rejection does not always cause noticeable symptoms. In fact, sometimes the only way rejection is detected is from routine blood tests. Some of the more common signs and symptoms of rejection include:
fever
headache
fatigue
nausea
loss of appetite
itchy skin (pruritus)
dark-coloured urine
jaundice (a yellowing of the skin and whites of the eyes)
abdominal tenderness or swelling
Acute liver rejection may occur in up to 10% of liver transplant recipients. It’s most common within the first three months after transplantation, but can occur at any time. To prevent rejection, you must take immunosuppressive medications for the rest of your life. These may include:
Prednisone
Tacrolimus (Prograf)
Cyclosporine (Sandimmune, Neoral)
Sirolimus (Rapamune)
Mycophenolate mofetil (CellCept)
The dose of these medications may change frequently, depending on your response. Generally, you can expect to take more medications the first few months following transplantation after which time some may be discontinued or the doses lowered.
The goal is to maintain a balance between preventing rejection and making you susceptible to infection and other side effects associated with the long-term use of immunosuppressant
Immediately after your transplant, we focus on:
Monitoring liver function and signs of rejection.
Adjusting your immunosuppressive medications
Recovery and rehabilitation
Return to Normalcy/Work
Most people are able to return to work within two to three months but Avoid lifting anything that weighs more than 10 lbs during this wound recovery. Usually your doctor won’t allow to drive usually during this time
Follow up
You will be expected to attend clinic once or twice a week first two months where we will do blood tests and adjust your liver medications and gradually distance between your follow up visits will increase. Stay in touch with your healthcare team if you have any concerns or questions.
Compliance
is the biggest issue particularly in kids in post-transplant care. As we know that after liver transplantation, one should take lifelong medications called Immunosuppressant.
Take your medications as advised.
Do not the skip the dose.
Protect yourself from common infections such as viruses and food poisoning.
Watch for signs of infection, such as fever, vomiting or swelling, and seek treatment right away.
Maintain a healthy diet and lifestyle. Try to get a little exercise most days.
This new normal require you to have stick to your follow up appointment, taking your medication regularly. It will take some time to adjust with this new environment, but you will have near normal life.
People with transplant is leading a normal life, getting back to their job, having a family, running a marathon and much more….
When we put a new liver in, we want new liver to work forever as liver in normal healthy individual does.
But it’s difficult to predict how long any given individual can be expected to live because of multiple reasons like
Age.
Overall health status.
recurrence of disease which can harm their new liver, usually take long time.
some patients go back to drinking habit again and start damaging their liver.
Non-compliance to medications may lead to rejection and graft loss.
The success rate for the transplant surgery itself is between 85% and 90%. That means the transplant was successful, the new liver was functional and the patient survived at one year.
The average survival rate after liver transplant is 75% after five years and 53% after 20 years.
Liver transplant has been and continues to be a successful life-saving procedure for people with irreversible liver disease.
Best centre
Best outcome
Best success rate
Best patient experience
All have one common answer
Your outcome depends on how comprehensive and experienced your team is.
You have to understand that liver transplant is not a one-person job. There are many health care providers involved in your transplant process. Do your research or ask upfront about it.
The success rate for the transplant surgery itself is between 85% and 90%.
There is no one answer to it.
I usually divide cost of transplant into three categories which varies between centres.
Pre transplant evaluation of donor and recipient cost around 1 to 1.5 lacks
Actual transplant surgery cost varies between 18 to 25 lacks.
And then post-transplant follows up cost which includes
- Cost of recurrent admissions after discharge:
- These admissions may be due to complications related to transplants like infections, rejections, bile duct issues, persistent fluid in the belly.
- Cost of post-transplant medications
- Cost of Blood tests and other imaging depending on your clinical conditions
That is around 10- 15 k per month for life time.