A pancreas transplant is a surgical procedure to place a healthy pancreas from a deceased donor into a person whose pancreas no longer functions properly.
The pancreas is an organ that lies behind the lower part of the stomach. One of its main functions is to make insulin, a hormone that regulates the absorption of sugar into cells.
If the pancreas doesn’t make enough insulin, blood sugar levels can rise to unhealthy levels, resulting in type 1 diabetes.
Most pancreas transplants are done to treat type 1 diabetes. It is often done in conjunction with a kidney transplant in people whose kidneys have been damaged by diabetes.
A pancreas transplant can restore insulin production and improve blood sugar control in people with diabetes, but it’s not a standard treatment. The side effects of the anti-rejection medications required after a pancreas transplant can often be serious.
Common indications:
Type 1 diabetes that cannot be controlled with standard treatment
Frequent insulin reactions
Consistently poor blood sugar control
Severe kidney damage
Type 2 diabetes associated with both low insulin resistance and low insulin production
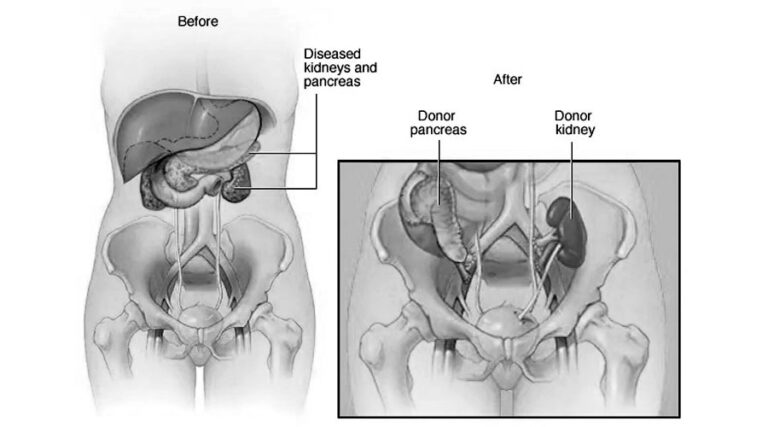
Pancreas transplant alone. People with diabetes and early or no kidney disease may be candidates for a pancreas transplant alone. A pancreas transplant surgery involves the placement of a healthy pancreas into a recipient whose pancreas is no longer functioning properly.
Combined kidney-pancreas transplant. Surgeons often may perform combined (simultaneous) kidney-pancreas transplants for people with diabetes who have or are at risk of kidney failure. Most pancreas transplants are done at the same time as a kidney transplant. The goal of this approach is to give you a healthy kidney and pancreas that are unlikely to contribute to diabetes-related kidney damage in the future.
Pancreas-after-kidney transplant. For those facing a long wait for both a donor kidney and a donor pancreas to become available, a kidney transplant may be recommended first if a living- or deceased-donor kidney becomes available. After you recover from kidney transplant surgery, you’ll receive a pancreas transplant once a donor pancreas becomes available.
Pancreatic islet cell transplant. During pancreatic islet cell transplantation, insulin-producing cells (islet cells) taken from a deceased donor’s pancreas are injected into a vein that takes blood to your liver. More than one injection of transplanted islet cells may be needed. Islet cell transplantation is being studied for people with serious, progressive complications from type 1 diabetes. It may only be performed as part of a Food and Drug Administration-approved clinical trial.